What is Glaucoma ?
Glaucoma is a term describing a group of ocular (eye) disorders that result in optic nerve damage, often associated with increased fluid pressure in the eye (intraocular pressure) (IOP).
The disorders can be roughly divided into two main categories:
- Open-angle glaucoma
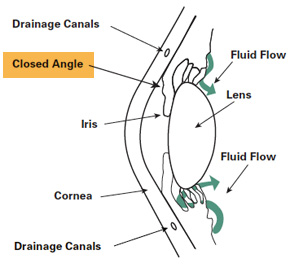
- Closed-angle(or angle closure) glaucoma
Open-angle chronic glaucomais painless, tends to develop slowly over time, and often has no symptoms until the disease has progressed significantly. It is treated by the eye specialist in Nagpur at SEH with either glaucoma medication to lower the pressure, or with various pressure-reducing glaucoma surgeries.
Closed-angle chronic glaucoma,however, is characterized by sudden eye pain, redness, nausea and vomiting, and other symptoms resulting from a sudden spike in intraocular pressure, and is treated as a medical emergency.
Glaucoma can permanently damage vision in the affected eye(s), first by decreasing peripheral vision (reducing the visual field), and then potentially leading to blindness if left untreated.


Classification Of Glaucoma
Primary open-angle glaucoma, also known as chronic open-angle glaucoma, chronic simple glaucoma, glaucoma simplex
- High-tension glaucoma
- Low-tension glaucoma
Primary angle closure glaucoma, also known as primary closed-angle glaucoma, narrow-angle glaucoma, pupil-block glaucoma, acute congestive glaucoma
- Acute angle closure glaucoma (aka AACG)
- Chronic angle closure glaucoma
- Intermittent angle closure glaucoma
- Superimposed on chronic open-angle closure glaucoma ("combined mechanism" – uncommon)
Variants of primary glaucoma
- Pigmentary glaucoma
- Exfoliation glaucoma, also known as pseudoexfoliative glaucoma or glaucoma capsulare
- Intermittent angle closure glaucoma
- Primary juvenile glaucoma
Developmental glaucoma
- Primary congenital glaucoma
- Infantile glaucoma
- Glaucoma associated with hereditary of familial diseases

Inflammatory glaucoma
- Uveitis of all types
- Fuchs heterochromic iridocyclitis
Phacogenic glaucoma
- Angle-closure glaucoma with mature cataract
- Phacoanaphylactic glaucoma secondary to rupture of lens capsule
- Phacolytic glaucoma due to phacotoxic meshwork blockage
- Subluxation of lens
- Glaucoma secondary to intraocular hemorrhage
- Hyphema
- Angle recession glaucoma: Traumatic recession on anterior chamber angle
- Postsurgical glaucoma
- Aphakic pupillary block
- Corticosteroid induced glaucoma
- Associated with intraocular tumors
- Associated with retinal detachments
- Secondary to severe chemical burns of the eye
- Associated with es
- sential iris atrophy
- Toxic glaucoma
Absolute glaucoma is the end stage of all types of glaucoma. The eye has no vision, absence of pupillary light reflex and pupillary response, and has a stony appearance. Severe pain is present in the eye. The treatment of absolute glaucoma is a destructive procedure like cyclocryoapplication, cyclophotocoagulation, or injection of 99% alcohol
The main symptom of glaucoma is gradual loss of vision. It is important to have regular eye tests to check for glaucoma later in life, especially if there is a family history of the condition.
Different types of glaucoma affect vision in different ways:
Chronic open-angle glaucoma
- Loss of peripheral field vision happens first, but because the peripheral field loss of open-angle glaucoma happens so gradually, the individual usually does not notice. That is why it is so important to have regular eye examinations by an eye doctor in Nagpur at Sood Eye Hospital, particularly if you have any risk factors.
Acute-angle closure glaucoma
- Sudden onset of throbbing pain and redness in the eye, headaches, blurred vision, halos around lights, a dilated pupil and sometimes nausea and vomiting.
- This type of glaucoma is a medical emergency and should be treated immediately. If not treated, it may result in severe permanent loss of vision or blindness.
Developmental (congenital) glaucoma in infants
- Tearing (watery eyes), sensitivity to light, and eyelid spasm are the three primary signs of congenital glaucoma.
- A larger cornea and clouding of the normally transparent cornea may also be noticed.
- The baby may habitually rub the eyes, squint or keep the eyes closed much of the time.
- If you notice any of these symptoms you should consult your GP or an optician as soon as possible.
Secondary and other forms of glaucoma
- Symptoms will depend on the underlying condition contributing to the abnormal rise in pressure. Inflammation inside the eye (uveitis) frequently causes halos and light sensitivity (photophobia). Injured eyes may mask glaucoma symptoms if eye damage (corneal oedema, bleeding, retinal detachment etc) is already present.
- If a cataract is the cause, vision will have been markedly reduced for a long time. Doctors managing complicated eye conditions in patients will monitor the intraocular pressure in order to detect the earliest pressure rise.
Of the several causes for glaucoma, ocular hypertension (increased pressure within the eye) is the most important risk factor in most glaucoma, but in some populations, only 50% of people with primary open-angle glaucoma actually have elevated ocular pressure.
No clear evidence indicates vitamin deficiencies cause glaucoma in humans. It follows, then, that oral vitamin supplementation is not a recommended treatment for glaucoma Caffeine increases intraocular pressure in those with glaucoma, but does not appear to affect normal individuals.
Many people of East Asian descent are prone to developing angle closure glaucoma due to shallower anterior chamber depths, with the majority of cases of glaucoma in this population consisting of some form of angle closure Inuit also have a 20- to 40-times higher risk of developing primary angle closure glaucoma. Women are three times more likely than men to develop acute angle closure glaucoma due to their shallower anterior chambers. People of African descent are three times more likely to develop primary open-angle glaucoma.
- Positive family history is a risk factor for glaucoma. The relative risk of having primary open-angle glaucoma (POAG) is increased about two- to four-fold for individuals who have a sibling with glaucoma.
- Glaucoma, particularly primary open-angle glaucoma, is associated with mutations in several different genes (including MYOC, ASB10, WDR36, NTF4, and TBK1 genes), although most cases of glaucoma do not involve these genetic mutations.
- Normal-tension glaucoma, which comprises one-third of POAG, is also associated with genetic mutations (including OPA1 and OPTN genes).
- Various rare congenital/genetic eye malformations are associated with glaucoma. Occasionally, failure of the normal third-trimester gestational atrophy of the hyaloid canal and the tunica vasculosa lentis is associated with other anomalies. Angle closure-induced ocular hypertension and glaucomatous optic neuropathy may also occur with these anomalies, and has been modeled in mice.
Other factors can cause glaucoma, known as "secondary glaucoma", including prolonged use of steroids (steroid-induced glaucoma); conditions that severely restrict blood flow to the eye, such as severe diabetic retinopathy and central retinal vein occlusion (neovascular glaucoma); ocular trauma (angle-recession glaucoma); and uveitis (uveitic glaucoma).
Based on the eye health condition, plethora of options is offered for glaucoma treatment in Nagpur at our hospital.
Intraocular pressure can be lowered with medication, usually eye drops. Several different classes of medications are used to treat glaucoma, with several different medications in each class.
Each of these medicines may have local and systemic side effects. Adherence to medication protocol can be confusing and expensive; if side effects occur, the patient must be willing either to tolerate them, or to communicate with the treating physician to improve the drug regimen. Initially, glaucoma drops may reasonably be started in either one or in both eyes
Poor compliance with medications and follow-up visits is a major reason for vision loss in glaucoma patients. A 2003 study of patients in an HMO found half failed to fill their prescriptions the first time, and one-fourth failed to refill their prescriptions a second time.[52] Patient education and communication must be ongoing to sustain successful treatment plans for this lifelong disease with no early symptoms.
The possible neuroprotective effects of various topical and systemic medications are also being investigated.
- Prostaglandin analogs, such as latanoprost (Xalatan), bimatoprost (Lumigan) and travoprost (Travatan), increase uveoscleral outflow of aqueous humor. Bimatoprost also increases trabecular outflow.
- Topical beta-adrenergic receptor antagonists, such as timolol, levobunolol (Betagan), and betaxolol, decrease aqueous humor production by the ciliary body.
- Alpha2-adrenergic agonists, such as brimonidine (Alphagan) and apraclonidine, work by a dual mechanism, decreasing aqueous humor production and increasing uveoscleral outflow.
- Less-selective alpha agonists, such as epinephrine, decrease aqueous humor production and increasing uveoscleral outflow.
- Less-selective alpha agonists, such as epinephrine, decrease aqueous humor production through vasoconstriction of ciliary body blood vessels, useful only in open-angle glaucoma. Epinephrine's mydriatic effect, however, renders it unsuitable for closed-angle glaucoma due to further narrowing of the uveoscleral outflow (i.e. further closure of trabecular meshwork, which is responsible for absorption of aqueous humor).
- Miotic agents (parasympathomimetics), such as pilocarpine, work by contraction of the ciliary muscle, opening the trabecular meshwork and allowing increased outflow of the aqueous humour. Echothiophate, an acetylcholinesterase inhibitor, is used in chronic glaucoma.
- Carbonic anhydrase inhibitors, such as dorzolamide (Trusopt), brinzolamide (Azopt), and acetazolamide (Diamox), lower secretion of aqueous humor by inhibiting carbonic anhydrase in the ciliary body.
When Is Glaucoma Surgery Needed?
Depending on the type of glaucoma you have, different treatment options may be considered. Non-surgical options include the use of topical eye medications (glaucoma eye drops) or oral medications (pills).
Most cases of glaucoma are controlled with one or more drugs by our hospital’s glaucoma specialist in Nagpur. But some people may require surgery to reduce their IOP further to a safe level by improving the outflow or drainage of fluids. Occasionally, surgery can eliminate the need for glaucoma eye drops. However, you may need to continue with eye drops even after having glaucoma surgery.
Some recent studies indicate that a laser procedure known as selective laser trabeculoplasty (SLT) may be equally as effective as glaucoma eye drops for lowering internal eye pressure. This laser surgery might be considered a primary treatment, particularly for people who find it difficult to comply with the strict, regular schedule needed for administering eye drops.
Another procedure called a trabeculectomy creates an artificial drainage area. This method is used in cases of advanced glaucoma where optic nerve damage has occurred and the IOP continues to soar. A third common option is a shunt, a device that a surgeon implants in your eye to improve fluid drainage.
Based on the medical feasibility and affordability of glaucoma surgery cost in Nagpur at our clinic, you can also opt for the best route in consultation with our eye specialists.
Laser Trabeculoplasty
- To increase outflow of internal eye fluid, an ophthalmologist performs laser trabeculoplasty with a laser that creates tiny holes in the filtration angle of the eye, where the cornea and iris meet.
- A newer procedure, selective laser trabeculoplasty, creates minimal heat damage to adjacent tissue, which generally means the procedure can be repeated safely.
- Laser trabeculoplasties are usually performed as an adjunct to a patient's ongoing eye drop therapy.
- Studies are now investigating whether SLT could be used routinely as a first-line therapy for treatment ofopen-angle glaucoma and other types of glaucoma, even before eye drops are used.
Trabeculectomy, Trabeculotomy and Goniotomy
- Glaucoma specialist in Nagpur at our clinic may recommend that a surgical incision be made into the eye's drainage system to create new channels for more normal flow of fluid. To accomplish this goal, a trabeculectomy involves partial removal of the eye's drainage system.
- Trabeculectomy is the most common surgical non-laser procedure performed for glaucoma when the IOP is no longer controlled by eye drops, pills or laser trabeculoplasties.
- Glaucoma surgery creates a new opening for fluid drainage. Graphic (enhanced) courtesy of National Eye Institute, National Institutes of Health.
- A trabeculectomy creates a "controlled" leak of fluid (aqueous humor) from the eye, which percolates under the conjunctiva. A small conjunctival "bleb" (bubble) appears at the junction of the cornea and the sclera (limbus) where this surgically produced valve is made.
- A trabeculotomy is the same as a trabeculectomy, except that incisions are made without removal of tissue.
- A goniotomy typically is used for infants and small children, when a special lens is needed for viewing the inner eye structures to create openings in the trabecular meshwork to allow drainage of fluids.
Iridotomy and Iridectomy
- In an iridotomy, a laser is used to create a hole in the iris to enhance the drainage passages blocked by a portion of the iris.
- An iridectomy involves surgically removing a small piece of the iris that will allow a better flow of fluid in eyes with narrow-angle glaucoma.
Shunts and Implants for Glaucoma
- Glaucoma shunts and stents are small devices that are surgically inserted into the eye during a trabeculectomy to increase outflow of intraocular fluid and reduce high eye pressure. The devices, usually made of materials such as silicone, polypropylene or biocompatible metals, create an alternative passageway for
- The term "glaucoma implants" sometimes is used to describe shunts and stents, but also describes tiny devices implanted in the eye that are designed to provide a sustained release of glaucoma medicine to reduce eye pressure.
- Complications of these implants can include creating a pressure that is too low for the eye to function (hypotony). Implants also can be positioned too close to the front of the eye's surface, causing corneal erosion. They also can cause erosions in the eye tissues where they have been placed.
Despite these risks, shunts and implants for glaucoma typically are safe and effective and can decrease or eliminate the need for daily glaucoma medications.
The SOLX DeepLight Glaucoma Treatment System combines a titanium sapphire laser with a gold shunt (shown at far left next to a quarter and at right inserted into an eye). At lower left and right are photos of a patient's trabecular meshwork before and after treatment.
Shunts and implants that have gained FDA approval for glaucoma surgery in the U.S. or that currently are in clinical trials include:
- Ex-Press Glaucoma Filtration Device- Offered by Alcon, this is a miniature, stainless steel shunt for glaucoma surgery that has been FDA-approved since 2002. About the size of a grain of rice, the Ex-Press shunt is implanted under a small flap created in the sclera and allows the aqueous to bypass the damaged trabecular meshwork and exit the eye more freely to lower IOP.
- In a study published in early 2012 that compared implantation of the Ex-Press Glaucoma Filtration Device with conventional trabeculectomy surgery, both procedures provided similar IOP control, but the Ex-Press group had a lower rate of complications and needed less glaucoma medication after surgery. DeepLight Glaucoma Treatment System- Developed by SOLX, the DeepLight Glaucoma Treatment System combines the use of titanium sapphire laser energy to open up the filtration angle of the eye and insertion of a hollow gold micro-shunt. The shunt creates an artificial channel to enable fluid drainage and relieve eye pressure. The laser and the shunt also can be used separately.
- The SOLX laser system, which received FDA approval in September 2008, is similar to selective laser trabeculoplasty (SLT), in that only pigmented cells are targeted, sparing adjacent tissue from potential heat damage. The DeepLight Gold Micro-Shunt operates differently from other types of glaucoma implants, because drainage is confined to the eye's interior with the idea of reducing surgical complications.
- The combined system has CE mark certification for use in Europe and currently is undergoing FDA clinical trials in the United States. iStent Trabecular Micro-Bypass- This shunt system from Glaukos Corp. is available in Europe for the treatment of open-angle glaucoma. The device also is commercially available in the United States and Canada for use in conjunction with cataract surgery for the reduction of IOP in patients with mild to moderate open-angle glaucoma.
- Made of surgical-grade titanium, the stent is placed in an internal area of the eye known as Schlemm's canal to re-establish a more normal flow of fluids within the eye.
- Durasert- In June 2011, pSividia Corp. announced an early stage clinical trial of its Durasert glaucoma implant is underway in the United States. The bioerodible implant is inserted under the scleral conjunctiva and is designed to provide long-term sustained release of the glaucoma medicine latanoprost, reducing or eliminating the need for daily medicated eye drops to treat glaucoma.
- CyPass Micro-Stent - In July 2011, Transcend Medical announced it had secured additional funding for a large U.S. clinical study and ongoing international trials of its CyPass Micro-Stent device.
- The CyPass device is designed to be inserted in the eye during routine cataract surgery for cataract patients who also have open angle glaucoma. More information about the U.S. clinical study of the device is available on the COMPASS Clinical Study website.
- Hydrus Microstent. This tiny implant, being developed by Ivantis, is roughly the size of an eyelash and is being tested in the U.S. for the treatment of primary open-angle glaucoma.
- The Hydrus procedure is less invasive than traditional glaucoma surgery and can be performed during cataract surgery using the same microsurgical incisions, according to the company.
- At the 2012 annual meeting of the American Academy of Ophthalmology, Thomas Samuelson, MD, reported first-year results of a Phase 3 FDA trial of the device, which revealed that glaucoma patients undergoing the Hydrus procedure required 69 percent less medication to control their eye pressure after the surgery.
- As a part of glaucoma treatment in Nagpur at SEH, non-penetrating glaucoma surgery is also suggested in few cases. Various innovative surgical techniques are carried out to alter the eye's drainage channels, improving the flow of fluids with only minimal penetration into the eye. These surgical methods involve superficial incisions that do not penetrate the eye as deeply as, for example, a trabeculectomy. Proponents say fewer complications are likely to result from these less invasive procedures.
- A deep sclerectomy involves a minimally invasive incision into the white of the eye (sclera), a portion of which is removed to create a drainage space for relief of eye pressure. A new surgical method known as viscocanalostomy creates an opening for insertion of a highly pliable, gel-like material known as viscoelastic, which helps provide enough space for adequate drainage and eye pressure relief.
- Glaucoma specialist in Nagpur and other cities across the world have differing viewpoints about the use of drug, laser, and surgical intervention to control high IOP. Although glaucoma surgery cost in Nagpur at our clinic is quite affordable, some glaucoma specialists, for example, say that long-term costs of drug treatments involving eye drops can be an economic burden that may be offset with the use of laser treatments.
- Others argue that treatments such as eye drops are far less invasive, are generally effective, and have fewer risks of complications than laser or non-laser surgical approaches. Study results comparing long-term effectiveness of different treatments also vary.
Treatment Cost
For cost of the treatment please fill our “ Quick Enquiry ” form given at the bottom of this page.
Sood Eye Hospital for Advance Eye Care Pvt.Ltd. is a World Class Facility Focused, 360 degree Quality Eye Care Hospital. Book Your Appointment Today !

