Cornea
The cornea is the transparent front part of the eye that covers the iris, pupil, and anterior chamber. The cornea, with the anterior chamber and lens, refracts light, with the cornea accounting for approximately two-thirds of the eye's total optical power.

Cornea - Services and Procedures
Cornea Services
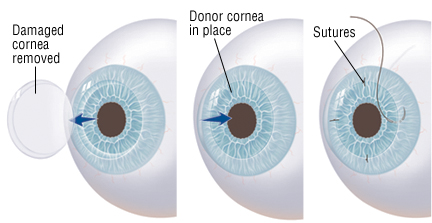
Corneal transplantation, also known as corneal grafting, is a surgical procedure conducted by our cornea specialist in Nagpur in which a damaged or diseased cornea is replaced by donated corneal tissue (the graft) in its entirety (penetrating keratoplasty) or in part (lamellar keratoplasty). (Keratoplasty is surgery to the cornea.) The graft is taken from a recently deceased individual with no known diseases or other factors that may affect the viability of the donated tissue or the health of the recipient.
Indications for include the following :
- Optical: To improve visual acuity by replacing the opaque or distorted host tissue by clear healthy donor tissue. The most common indication in this category is pseudophakic bullous keratopathy, followed by keratoconus, corneal degeneration, keratoglobus and dystrophy, as well as scarring due to keratitis and trauma.
- Tectonic/reconstructive: To preserve corneal anatomy and integrity in patients with stromal thinning and descemetoceles, or to reconstruct the anatomy of the eye, e.g. after corneal perforation.
- Therapeutic: To remove inflamed corneal tissue unresponsive to treatment by antibiotics or anti-virals.
- Cosmetic: To improve the appearance of patients with corneal scars those have given a whitish or opaque hue to the cornea.

- In most instances, the patient will meet with their ophthalmologist for an examination in the weeks or months preceding the surgery. During the exam, our retina specialist in Nagpur at MSEH will examine the eye and diagnose the condition. The doctor will then discuss the condition of the patient, including the different treatment options available. The doctor will also discuss the risks and benefits of the various options.
- If the patient elects to proceed with the surgery for corneal disease treatment in Nagpur at our hospital, the doctor will have the patient sign an informed consent form. The doctor might also perform a physical examination and order lab tests, such as blood work, X-rays, or an EKG.
- The surgery date and time will also be set, and the patient will be told where the surgery will take place.

- On the day of the surgery, the patient arrives at MSEH, the best eye hospital in Nagpur, where the procedure will be performed. The patient is given a brief physical examination by the surgical team and is taken to the operating room. In the OR, the patient lies down on an operating table and is either given general anesthesia, or local anesthesia and a sedative.
- With anesthesia induced, the surgical team prepares the eye to be operated on and drapes the face around the eye. An eyelid speculum is placed to keep the lids open, and some lubrication is placed on the eye to prevent drying. In children, a metal ring is stitched to the sclera which will provide support of the sclera during the procedure.

- A trephine (a circular cutting device), which removes a circular disc of cornea, is used by the surgeon to cut the donor cornea. A second trephine is then used to remove a similar-sized portion of the patient's cornea. The donor tissue is then sewn in place with sutures.
- Antibiotic eye drops are placed, the eye is patched, and the patient is taken to a recovery area while the effects of the anesthesia wear off. The patient typically goes home following this and sees the doctor the following day for the first postoperative appointment.
- Lamellar keratoplasty encompasses several techniques which selectively replace diseased layers of the cornea while leaving healthy layers in place. The chief advantage is improved tectonic integrity of the eye. Disadvantages include the technically challenging nature of these procedures, which replace portions of a structure only 500 µm thick, and reduced optical performance of the donor/recipient interface compared to full-thickness keratoplasty.
- In this procedure, the anterior layers of the central cornea are removed and replaced with donor tissue. Endothelial cells and the Descemets membrane are left in place. While offering ocular surface disorder treatment in Nagpur by our eye surgeons, this technique is used in cases of anterior corneal opacifications, scars, and ectatic diseases such as keratoconus.
- Endothelial keratoplasty replaces the patient's endothelium with a transplanted disc of posterior stroma/Descemets/endothelium (DSEK) or Descemets/endothelium (DMEK).This relatively new procedure has revolutionized treatment of disorders of the innermost layer of the cornea (endothelium). Unlike a full-thickness corneal transplant, the surgery can be performed with one or no sutures. Patients may recover functional vision in days to weeks, as opposed to up to a year with full thickness transplants.
- However, an Australian study has shown that despite its benefits, the loss of endothelial cells that maintain transparency is much higher in DSEK compared to a full-thickness corneal transplant. The reason may be greater tissue manipulation during surgery, the study concluded.
- During surgery the patient's corneal endothelium is removed and replaced with donor tissue. With DSEK, the donor includes a thin layer of stroma, as well as endothelium, and is commonly 100–150 µm thick. With DMEK, only the endothelium is transplanted. In the immediate postoperative period the donor tissue is held in position with an air bubble placed inside the eye (the anterior chamber). The tissue self-adheres in a short period and the air is adsorbed into the surrounding tissues.
- Complications include displacement of the donor tissue requiring repositioning ("refloating"). This is more common with DMEK than DSEK. Folds in the donor tissue may reduce the quality of vision, requiring repair. Rejection of the donor tissue may require repeating the procedure. Gradual reduction in endothelial cell density over time can lead to loss of clarity and require repeating the procedure.
- Patients with endothelial transplants frequently achieve best corrected vision in the 20/30 to 20/40 range, although some reach 20/20. Optical irregularity at the graft/host interface may limit vision below 20/20.
- The risks are similar to other intraocular procedures, detachment or displacement of lamellar transplants. There is also a risk of infection. Since the cornea has no blood vessels (it takes its nutrients from the aqueous humor) it heals much more slowly than a cut on the skin. While the wound is healing, it is possible that it might become infected by various microorganisms. This risk is minimized by antibiotic prophylaxis (using antibiotic eye drops, even when no infection exists). There is a risk of cornea rejection, which occurs in about 20% of cases
- The prognosis for visual restoration and maintenance of ocular health with corneal transplants is generally very good. Risks for failure or guarded prognoses are multifactorial. The type of transplant, the disease state requiring the procedure, the health of the other parts of the recipient eye and even the health of the donor tissue may all confer a more or less favorable prognosis. The majority of corneal transplants result in significant improvement in visual function for many years or a lifetime. In cases of rejection or transplant failure, the surgery generally can be repeated.
- Descemet Membrane Endothelial Keratoplasty (DMEK) is the most recent EK technique in which an isolated Descemet membrane is transplanted. The DMEK procedure is a 'like for like' replacement of the diseased part of the cornea with visual rehabilitation to 20/40 or better in 90% of cases and 20/25 or better in 60% of cases within the first three months.
- Rejection rates are lower (1%) and visual recovery is faster than any other form of corneal transplantation. DMEK is available to patients for ocular surface disorder treatment in Nagpur at our clinic.
- There is a bioengineering technique that uses stem cells to create corneas or part of corneas that can be transplanted into the eyes. Corneal stem cells are removed from a healthy cornea. They are collected and, through laboratory procedures, made into five to ten layers of cells that can be stitched into a patient's eye. The stem cells are placed into the area where the damaged cornea tissue has been removed. This is a good alternative for those that cannot gain vision through regular cornea.

